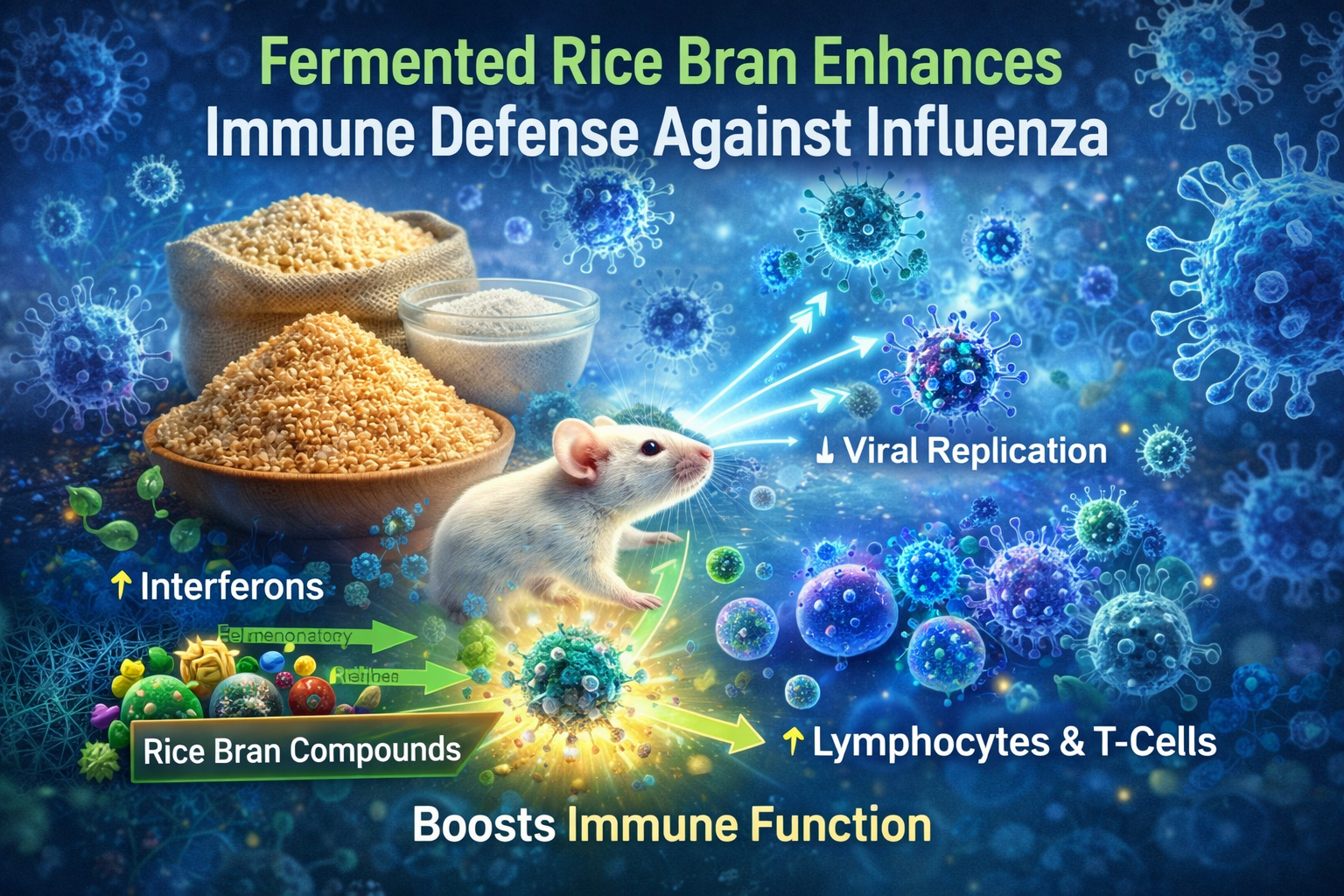
A groundbreaking study has revealed compelling evidence that fermented rice bran may play a powerful role in strengthening immune defenses and suppressing influenza virus activity. The research, led by K. Hayashi, explores the relationship between nutrition and viral infection, demonstrating that oral intake of fermented rice bran significantly reduces viral replication while enhancing immune function. Using both immunocompetent and immunocompromised mouse models infected with influenza, the study highlights the critical role of diet—and particularly gut microbiota—in shaping immune responses.
To ensure reliable results, researchers designed a carefully controlled experiment in which laboratory mice were categorized based on immune status. The primary objective was to assess whether a targeted dietary intervention could support or amplify immune defenses when faced with a widespread viral threat like influenza. Through systematic observation and detailed analysis, the research team generated strong evidence that fermented rice bran plays a meaningful role in limiting viral activity.
Rice bran, a natural byproduct of rice milling, contains a rich array of bioactive substances, including phenolic compounds, flavonoids, and dietary fibers. Fermentation enhances the accessibility and absorption of these nutrients, allowing the body to utilize them more effectively. The researchers proposed that these compounds could help regulate immune activity while directly interfering with viral replication. This hypothesis was rigorously evaluated through in vivo testing, yielding notable and consistent results.
One of the most significant outcomes was a substantial decrease in viral load among both immune-healthy and immune-compromised mice that received fermented rice bran. The antiviral effect appeared to result from multiple mechanisms, particularly the stimulation of interferon production—key signaling proteins that coordinate immune defense. Increased interferon activity not only slowed viral reproduction but also strengthened the host’s overall immune response.
Beyond viral suppression, fermented rice bran positively influenced several immune indicators. The study observed enhanced lymphocyte proliferation and increased cytokine production in supplemented mice. Critical immune cells, including T cells and B cells, showed heightened activity and numbers compared to control groups. These findings suggest that fermented rice bran functions as a true immune-supportive food, reinforcing the body’s ability to respond to viral challenges.
The results are especially meaningful for individuals with weakened immune systems. Immunocompromised populations are particularly vulnerable to severe complications from viral infections, and traditional treatments may offer limited protection. The ability of fermented rice bran to stimulate immune activity in these cases presents a promising nutritional strategy that could complement existing therapies and improve overall health outcomes.
The implications of this research extend well beyond laboratory findings. It lays a foundation for future clinical studies exploring dietary approaches to enhance antiviral immunity, particularly among high-risk groups such as older adults or patients undergoing immunosuppressive treatments. The use of natural, food-based interventions aligns with a growing emphasis on preventive and holistic healthcare rather than reliance solely on pharmaceutical solutions.
In their conclusions, the authors emphasize the need for further research to better understand the exact biological pathways through which fermented rice bran exerts its antiviral effects. Future investigations may focus on identifying specific microbial strains involved in fermentation and determining how they interact with the immune system. Such insights could lead to optimized formulations designed to maximize health benefits.
Overall, this study provides persuasive evidence that dietary strategies—specifically the inclusion of fermented rice bran—can serve as effective tools in combating viral infections like influenza. The findings support innovative approaches that integrate nutrition into both prevention and treatment frameworks aimed at strengthening immune resilience.
As awareness grows regarding the connection between diet and immune health, this research reinforces the idea that food can function as more than sustenance—it can actively support disease resistance. In an era marked by ongoing infectious threats, nutritional solutions are increasingly vital to public health strategies.
This research not only deepens our understanding of how nutrition influences immune defense but also challenges conventional views of dietary habits. Incorporating functional foods such as fermented rice bran into everyday diets may offer an accessible and sustainable line of protection against viral illnesses. As public health models continue to evolve, nutrition-focused prevention could become a central pillar of comprehensive healthcare.
Ultimately, these findings remind us of the profound link between dietary choices and immune performance. By illuminating the mechanisms through which food supports immune resilience, this study contributes to a broader shift toward sustainable, holistic health practices. Continued research may further refine personalized nutrition strategies, allowing individuals to optimize immune health based on their unique biological profiles.
In closing, this study underscores a growing truth in modern science: what we eat has a direct and meaningful impact on how our bodies respond to disease. The concept of food as medicine is gaining momentum, and evidence like this strengthens the case for nutrition-centered approaches in the ongoing fight against viral infections such as influenza.